Cholestatic liver diseases (ChLD) are chronic, progressive conditions that require urgent attention
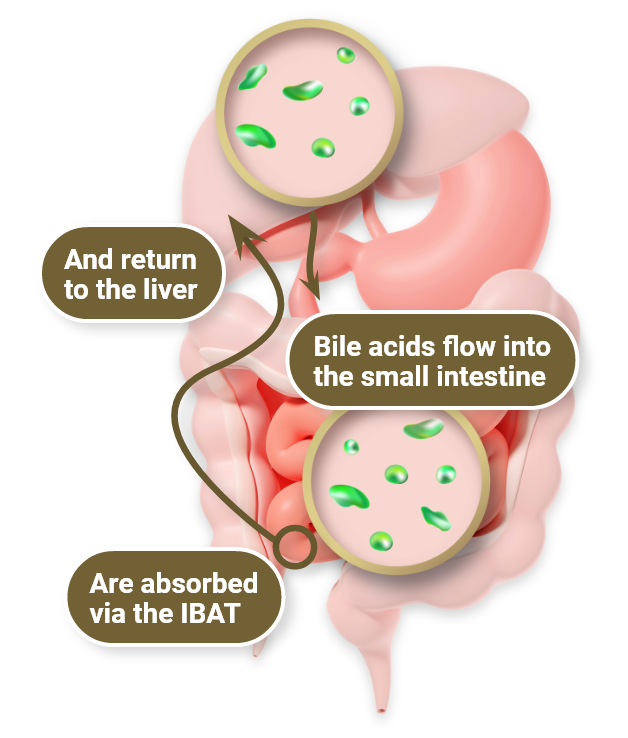
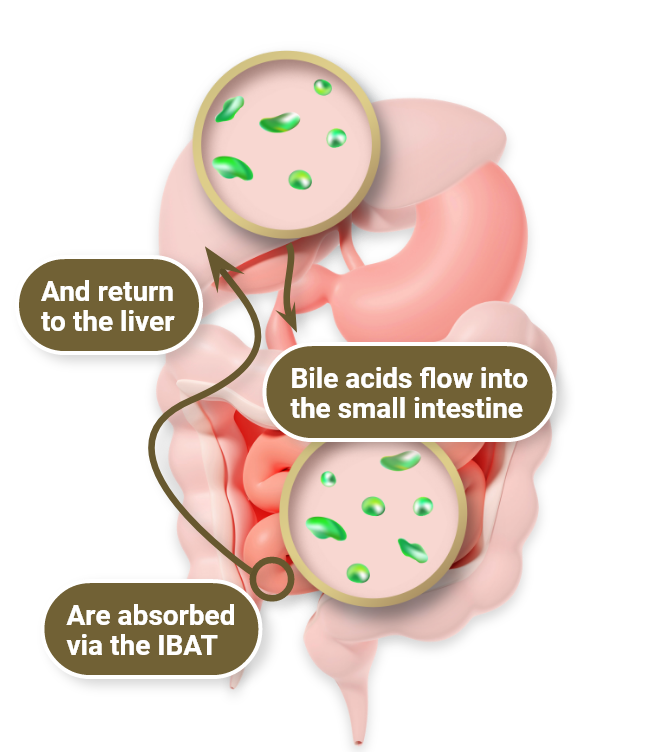
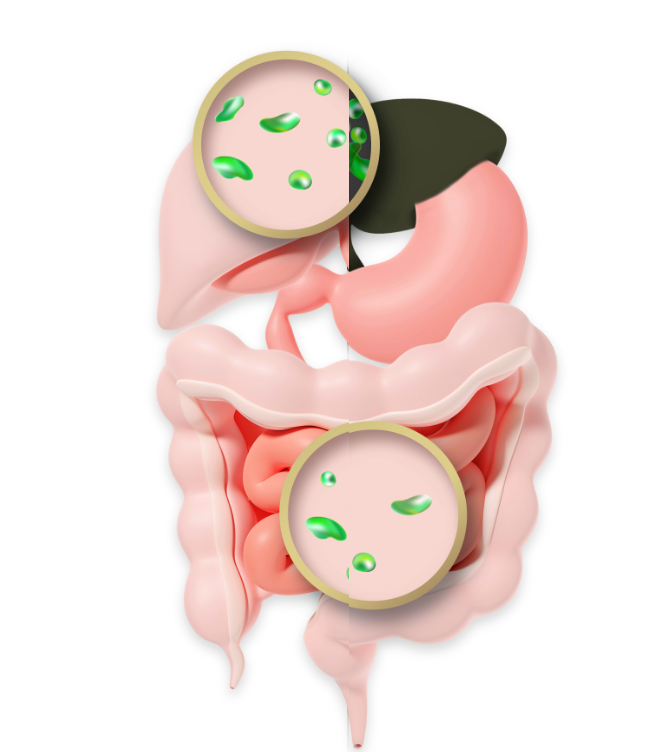
Healthy hepatic and gastrointestinal functions are dependent on proper bile formation and flow1,2
Bile acids serve 2 critical functions
-
Helping to dispose of metabolic waste products excreted in the liver1,9
-
Emulsifying nutritional lipids to facilitate digestion and absorption2
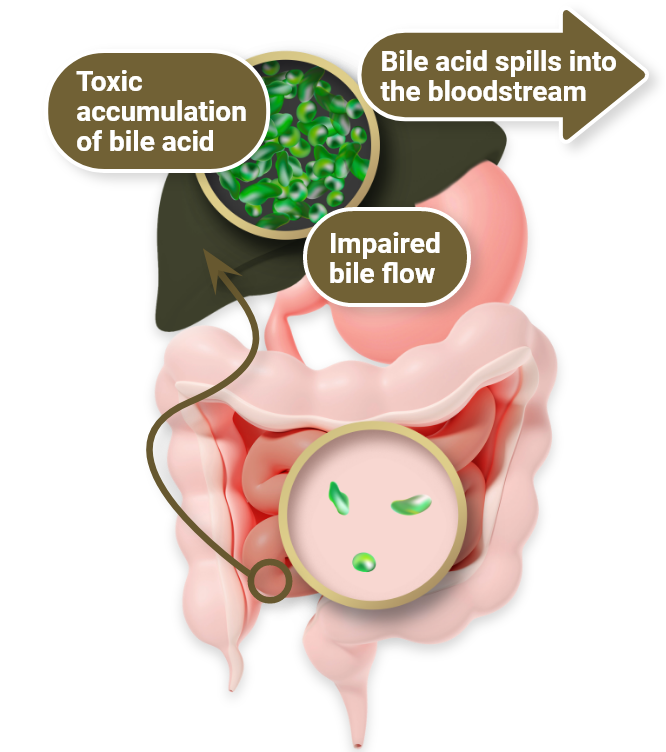
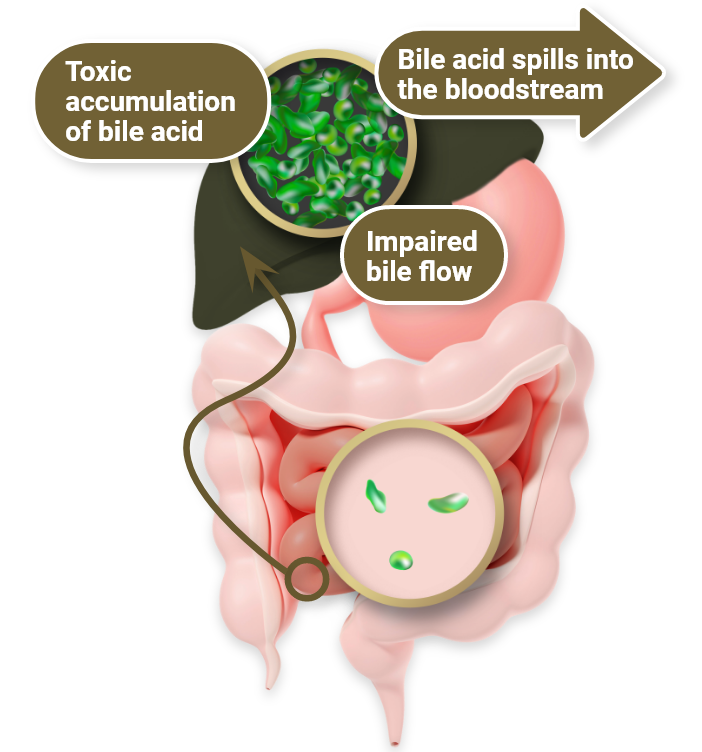
Chronic ChLD affects bile flow and can lead to a toxic accumulation in the liver
PFIC
Progressive familial intrahepatic cholestasis
PFIC results in disrupted hepatocyte and/or intrahepatic bile duct function and commonly presents in early infancy but can manifest later in life.2,3
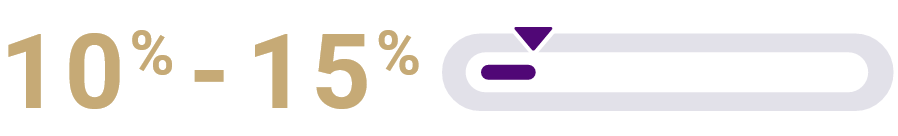
of all ChLD cases in children are PFIC, a heterogeneous group of rare, life-threatening, autosomal recessive cholestatic liver diseases.2,10
The estimated incidence of PFIC is 1 in every 50,000 to 100,000 births.3

In a retrospective analysis of 130 PFIC 1 patients from the NAPPED consortium, 44% of patients with PFIC 1 survived to age 18 with their native liver. Without surgery the likelihood of liver failure is high.11

In a retrospective analysis of 264 PFIC 2 patients from the NAPPED consortium, 32% of patients with PFIC 2 survived to age 18 with their native liver. Without surgery the likelihood of liver failure is high.12
ALGS
Alagille syndrome
ALGS is a rare, multisystem, autosomal-dominant, life-threatening disease caused by genetic mutations.8,13
It is one of most common forms of an inherited cholestatic liver disease in children.13
1 in every 30,000 to 45,000 individuals are estimated to have an ALGS diagnosis.14

In a retrospective analysis of 1,433 children with clinically and/or genetically confirmed ALGS, 40% of patients with ALGS survived to age 18 with their native liver.15
Untreated ChLD results in a variety of severe consequences for patients


Failure to thrive
Failure to thrive is a result of insufficient weight gain, delayed growth, and deficient bone health.5,8,14-20
Cholestasis affects the ability to absorb fat-soluble vitamins (FSV), leading to17,18
Malnutrition
Poor growth
FSV deficiency
Risk for
weakened
bone strength
Fracture

Surgical intervention
Diversion procedures can help improve symptoms and delay disease progression. But there are risks involved, and surgery may not completely resolve ChLD symptoms.10,21
Eventually, liver transplantation may be needed.10,14
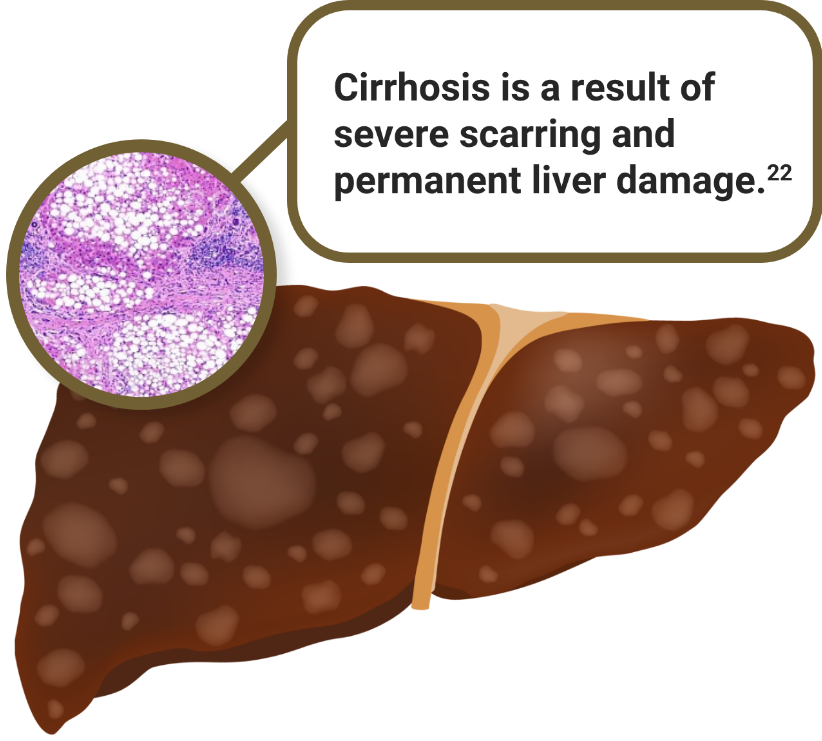
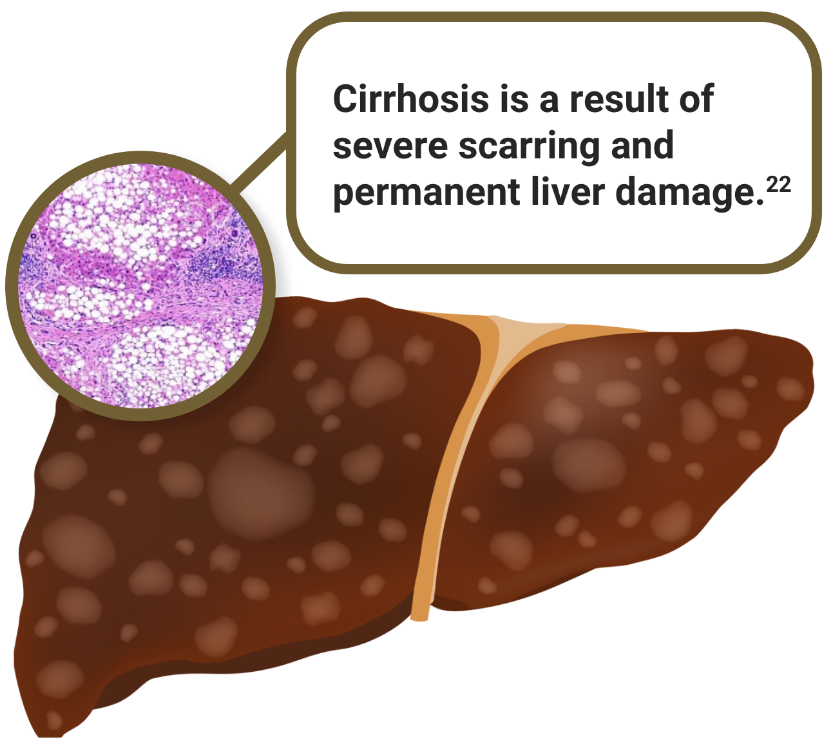
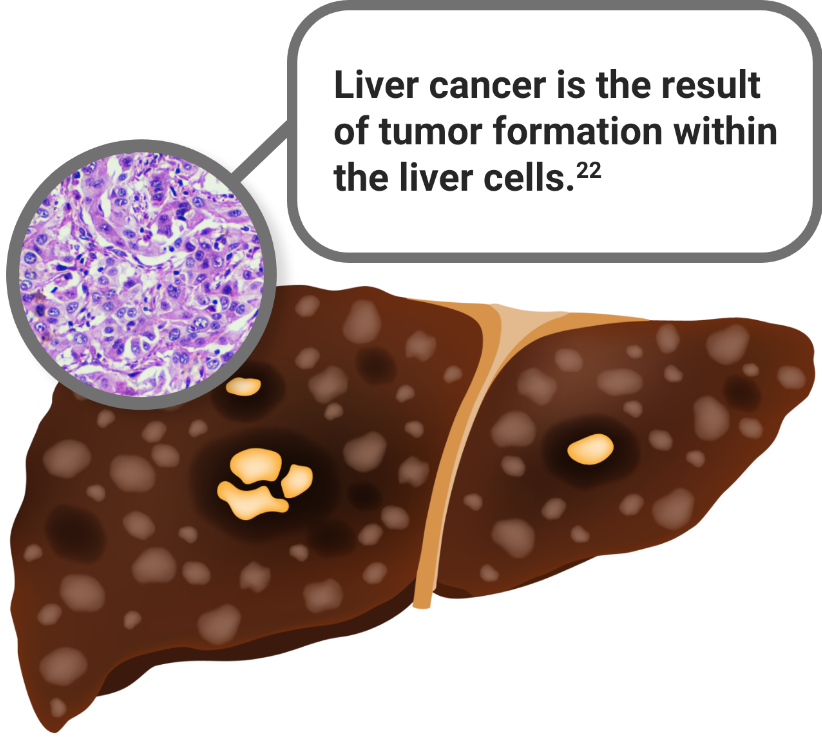
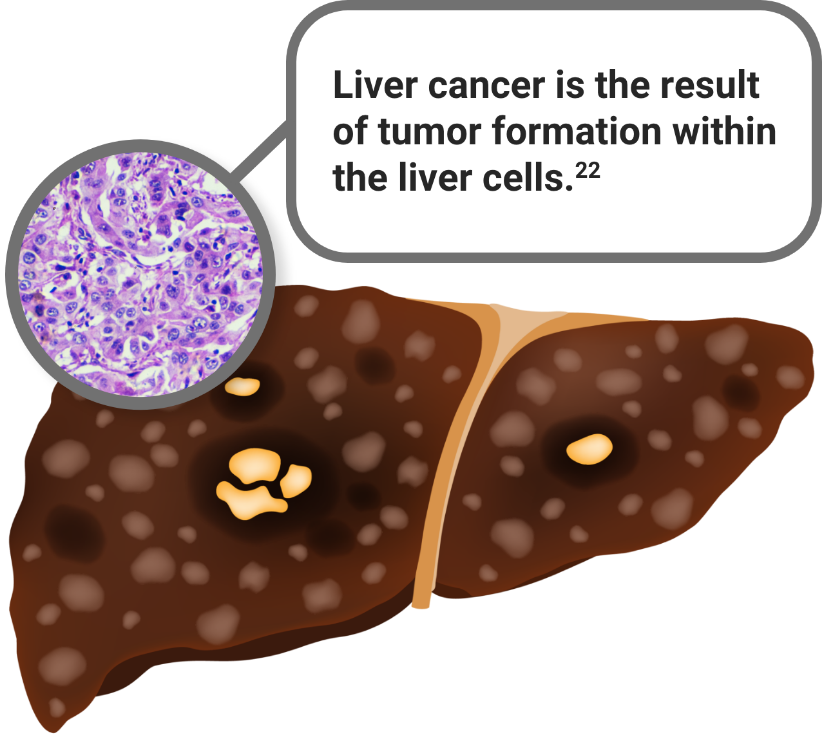
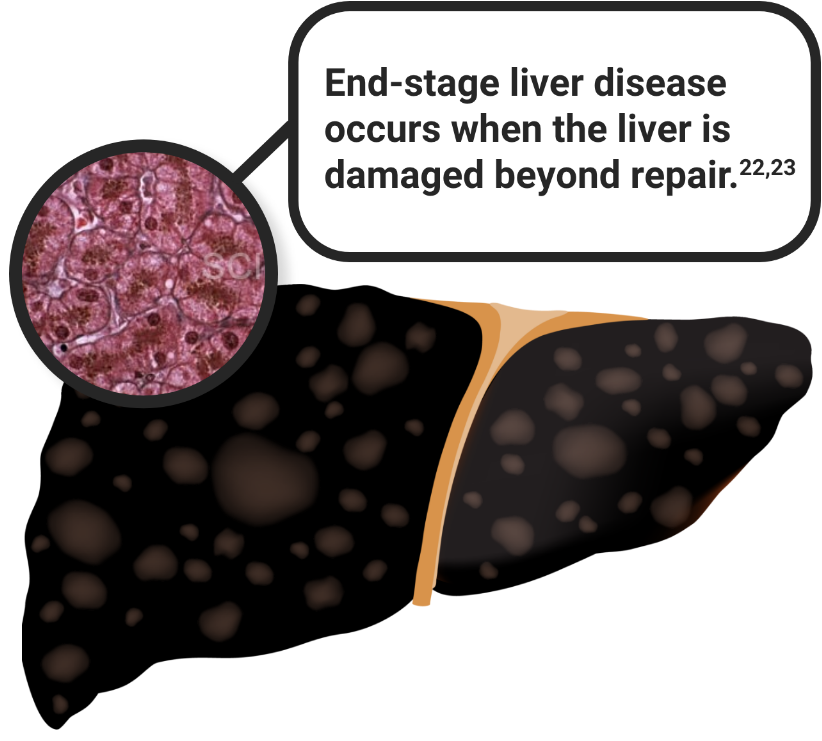
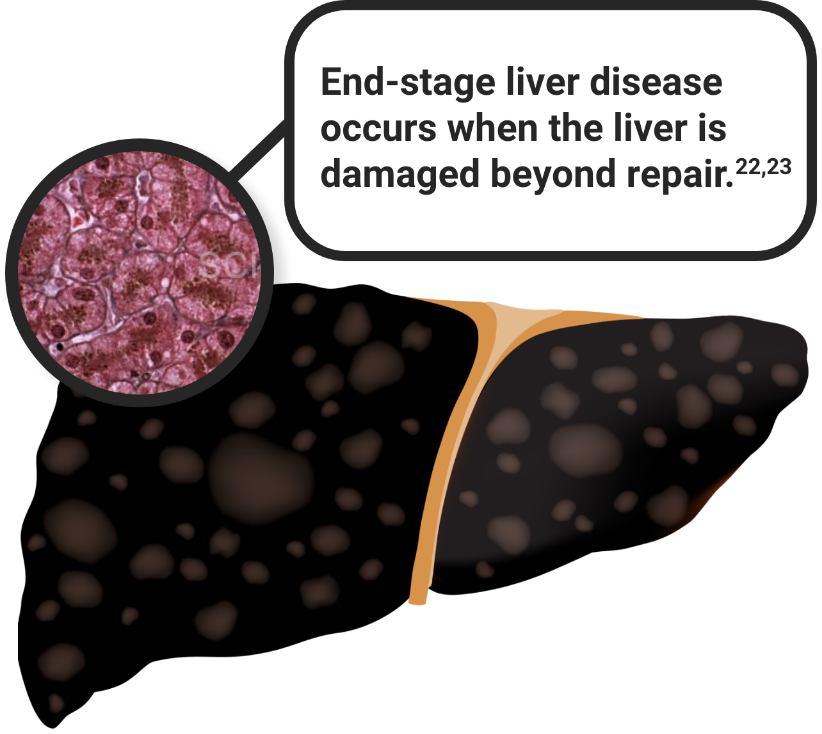
Irreversible progression
Irreversible progression of liver disease may lead to liver transplantation and possible fatal complications.
Fibrosis, cirrhosis, liver failure, and even death may occur if ChLD is not managed.2,5,6,8
Select a stage to see progression.




The first step to treating ChLD is identifying it early

ChLD=cholestatic liver diseases; NAPPED=NAtural course and Prognosis of PFIC and Effect of biliary Diversion.
References: 1. Bull LN, Thompson RJ. Progressive familial intrahepatic cholestasis. Clin Liver Dis. 2018;22(4):657-669. 2. Kamath BM, Stein P, Houwen RHJ, Verkade HJ. Potential of ileal bile acid transporter inhibition as a therapeutic target in Alagille syndrome and progressive familial intrahepatic cholestasis. Liver Int. 2020;40(8):1812-1822. 3. Davit-Spraul A, Gonzales E, Baussan C, Jacquemin E. Progressive familial intrahepatic cholestasis. Orphanet J Rare Dis. 2009;4:1. 4. Siddiqi I, Tadi P. Progressive familial intrahepatic cholestasis. StatPearls [Internet]. NCBI bookshelf. Accessed April 20, 2023. https://www.ncbi.nlm.nih.gov/books/NBK559317/ 5. Turnpenny PD, Ellard S. Alagille syndrome: pathogenesis, diagnosis, and management. Eur J Hum Genet. 2012;20(3):251-257. 6. Krantz ID, Piccoli DA, Spinner NB. Alagille syndrome. J Med Genet. 1997;34(2):152-157. 7. Mehl A, Bohorquex H, Serrano M-S, Galliano G, Reichman TW. Liver transplantation and the management of progressive familial intrahepatic cholestasis in children. World J Transplant. 2016;6(2):278-290. 8. Kamath BM, Baker A, Houwen R, Todorova L, Kerkar N. Systematic review: the epidemiology, natural history, and burden of Alagille syndrome. J Pediatr Gastroenterol Nutr. 2018;67(2):148-156. 9. Hofmann AF. Bile acids: the good, the bad, and the ugly. News Physiol Sci. 1999;14:24-29. 10. Gunaydin M, Bozkurter Cil AT. Progressive familial intrahepatic cholestasis: diagnosis, management, and treatment. Hepat Med. 2018;10:95-104. 11. van Wessel DBE, Thompson RJ, Gonzales E, et al. Impact of genotype, serum bile acids, and surgical biliary diversion on native liver survival in FIC1 deficiency. Hepatology. 2021;74(2):892-906. 12. van Wessel DBE, Thompson RJ, Gonzales E, et al. Genotype correlates with the natural history of severe bile salt export pump deficiency. J Hepatol. 2020;73(1):84-93. 13. Jeyaraj R, McKay Bounford K, Ruth N, et al. The genetics of inherited cholestatic disorders in neonates and infants: evolving challenges. Genes (Basel). 2021;12(11):1-20. 14. National Organization for Rare Disorders. Alagille syndrome. Updated May 13, 2020. Accessed February 22, 2023. https://rarediseases.org/rare-diseases/alagille-syndrome/?filter=ovr-ds-resources 15. Vandriel SM, Li L-T, She H, et al. Natural history of liver disease in a large international cohort of children with Alagille syndrome: results from the GALA study. Hepatology. 2023;77(2):512-529. 16. Johns Hopkins Medicine. Progressive Familial Intrahepatic Cholestasis. Accessed August 1, 2023. https://www.hopkinsmedicine.org/health/conditions-and-diseases/progressive-familial-intrahepatic-cholestasis 17. Yang CH, Perumpail BJ, Yoo ER, Ahmed A, Kerner JA Jr. Nutritional needs and support for children with chronic liver disease. Nutrients. 2017;9(10):1127. 18. Hilscher MB, Kamath PS, Eaton JE. Cholestatic liver diseases: a primer for generalists and subspecialists. Mayo Clin Proc. 2020;95(10):2263-2279. 19. The Childhood Liver Disease Research Network. Accessed August 1. https://childrennetwork.org/Clinical-Studies/Progressive-Familial-Intrahepatic-Cholestasis 20. Ayoub MD, Kamath BM. Alagille syndrome: diagnostic challenges and advances in management. Diagnostics (Basel). 2020;10(11):1-18. 21. Wang KS, Tiao G, Bass LM, et al. Analysis of surgical interruption of the enterohepatic circulation as a treatment for pediatric cholestasis. Hepatology. 2017;65(5):1645-1654. 22. American Liver Foundation. How liver diseases progress. Updated March 2, 2023. Accessed June 8, 2023. https://liverfoundation.org/about-your-liver/how-liver-diseases-progress/ 23. NHS Blood and Transplant. Accessed August 1, 2023. https://www.nhsbt.nhs.uk/organ-transplantation/liver/is-a-liver-transplant-right-for-you/end-stage-liver-disease/